Palliative Care Facts and Stats
March 5, 2025
Discover intriguing palliative care facts and stats that will reshape your understanding of this essential healthcare field.


Understanding Palliative Care
Diving into the realm of palliative care involves grasping the definition and purpose of this specialized form of medical care that focuses on enhancing the quality of life for patients facing serious illnesses. Let's delve into the core aspects that define palliative care and its significance in the healthcare landscape.

Definition and Purpose of Palliative Care
Palliative care is a holistic approach to healthcare that emphasizes providing relief from the symptoms and stress of a serious illness. It is tailored to meet the unique needs of each individual and their families, aiming to improve the overall quality of life. Palliative care is not limited to end-of-life situations but begins at the time of diagnosis and continues throughout the illness trajectory.
Importance of Palliative Care in Healthcare
The importance of palliative care in healthcare cannot be overstated. It plays a crucial role in addressing the physical, emotional, and spiritual needs of patients dealing with life-limiting conditions. By focusing on symptom management, pain relief, and enhancing comfort, palliative care helps patients and their families navigate the complexities of serious illnesses.
Moreover, integrating palliative care early in the treatment plan has been shown to improve patient outcomes, increase patient satisfaction, and reduce healthcare costs. This person-centered approach ensures that individuals receive the support they need to cope with the challenges of their illness while maintaining dignity and autonomy.
By understanding the fundamental principles and impact of palliative care, both healthcare providers and patients can make informed decisions that align with their values and preferences. This comprehensive approach underscores the profound impact that palliative care can have on individuals facing serious illnesses, fostering a compassionate and supportive healthcare environment.
Palliative Care Stats Overview
When exploring the landscape of palliative care, it's essential to delve into the statistics that shed light on its growth and utilization, as well as the demographics of patients benefiting from these services.
Growth and Usage of Palliative Care Services
Palliative care has witnessed a significant increase in utilization over the years, reflecting the growing recognition of its importance in enhancing quality of life for patients with serious illnesses. Here are some key statistics highlighting the growth and usage of palliative care services:
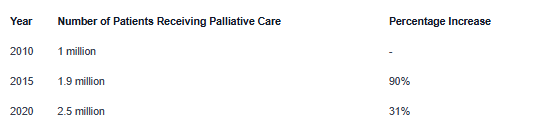
The data underscores the steady rise in the number of individuals benefitting from palliative care, showcasing the increasing acceptance and integration of these services within the healthcare system.
Demographics of Patients Receiving Palliative Care
Understanding the demographics of patients receiving palliative care is crucial for tailoring services to meet the diverse needs of individuals facing serious illnesses. Here is an overview of the demographics of patients accessing palliative care:

Additionally, studies have shown that there is a balanced distribution between male and female patients receiving palliative care, highlighting the inclusive nature of these services across different genders.
By examining the growth trends and demographic characteristics of individuals receiving palliative care, we gain valuable insights into the evolving landscape and the increasing importance of palliative care in providing holistic support to patients with serious illnesses.
Benefits of Palliative Care
Palliative care offers a holistic approach to supporting individuals with serious illnesses, focusing on enhancing their quality of life. Here are the key benefits of palliative care in managing symptoms and pain, improving quality of life, and supporting emotional well-being.
Managing Symptoms and Pain
Palliative care plays a crucial role in managing the symptoms and pain associated with serious illnesses. By providing specialized medical interventions and treatments, palliative care aims to alleviate discomfort and enhance the overall well-being of individuals.

Improving Quality of Life
One of the primary goals of palliative care is to improve the quality of life for individuals facing serious illnesses. By addressing physical, emotional, and spiritual needs, palliative care helps patients and their families cope with the challenges associated with the illness.

Supporting Emotional Well-being
In addition to physical symptoms, palliative care places a strong emphasis on supporting the emotional well-being of patients and their families. Through counseling, psychosocial support, and spiritual care, palliative care helps individuals navigate the complex emotional journey associated with serious illnesses.

By focusing on symptom management, improving quality of life, and providing emotional support, palliative care offers a multi-faceted approach to caring for individuals with serious illnesses. These benefits highlight the importance of integrating palliative care into standard healthcare practices to ensure comprehensive and compassionate support for patients and their families.
Palliative Care in Different Settings
Palliative care is provided in various settings to cater to the diverse needs of patients requiring such specialized care. The different settings for palliative care include hospital-based palliative care, home-based palliative care, and palliative care in long-term care facilities.
Hospital-Based Palliative Care
In a hospital setting, palliative care is often integrated into the comprehensive medical services offered to patients with serious illnesses. This approach ensures that individuals in hospitals receive holistic care focused on relieving symptoms, managing pain, and enhancing their quality of life. Hospital-based palliative care teams typically consist of healthcare professionals with expertise in palliative medicine, nursing, social work, and spiritual care.

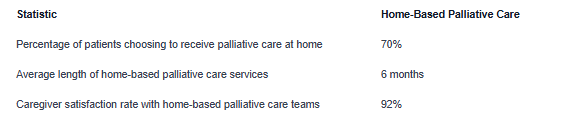
Home-Based Palliative Care
Home-based palliative care offers patients the opportunity to receive compassionate care in the comfort of their own homes. This setting allows individuals with advanced illnesses to remain in familiar surroundings while receiving symptom management, emotional support, and coordination of care. Home-based palliative care teams often include specialized nurses, physicians, social workers, and therapists who visit patients at home to provide personalized care.
Palliative Care in Long-Term Care Facilities
Palliative care services in long-term care facilities are tailored to meet the complex needs of residents living with chronic or terminal illnesses. By integrating palliative care principles into long-term care settings, individuals receive comprehensive support to enhance their quality of life and promote comfort. The interdisciplinary palliative care teams in these facilities collaborate closely with residents, families, and staff to address physical, emotional, and spiritual needs.

By offering palliative care in diverse settings such as hospitals, homes, and long-term care facilities, healthcare providers can ensure that individuals with serious illnesses receive personalized and compassionate care that aligns with their preferences and needs. Each setting plays a vital role in supporting patients and their families throughout their palliative care journey.
Challenges and Misconceptions
When it comes to palliative care, there are certain challenges and misconceptions that can impact the delivery and understanding of these vital services. In this section, we will explore two key areas: access to palliative care services and misunderstandings surrounding palliative care.
Access to Palliative Care Services
Access to palliative care services remains a significant challenge for many individuals, despite the benefits it offers. Limited availability of palliative care resources, especially in rural areas, can create barriers for patients in need of these specialized services. Additionally, factors such as lack of awareness among healthcare providers and patients, insufficient funding, and disparities in healthcare infrastructure can further hinder access to quality palliative care.
Ensuring equitable access to palliative care services requires collaborative efforts from healthcare organizations, policymakers, and advocacy groups. Strategies such as expanding palliative care programs, enhancing education and training for healthcare professionals, and advocating for improved reimbursement policies can help address the access barriers and ensure that more individuals receive the palliative care they deserve.
Misunderstandings Surrounding Palliative Care
Misconceptions about palliative care are prevalent and can prevent individuals from seeking these services at crucial stages of illness. One common misunderstanding is equating palliative care with end-of-life care only. In reality, palliative care focuses on providing holistic support to individuals with serious illnesses at any stage, emphasizing symptom management, emotional well-being, and quality of life enhancement.
Another misconception is the belief that palliative care is equivalent to giving up or forgoing curative treatment. Palliative care can be integrated alongside curative treatments and does not signify an end to active medical interventions. By dispelling these misconceptions and raising awareness about the benefits of palliative care, individuals can make more informed decisions about their care preferences and receive the support they need to enhance their overall well-being.
Through addressing challenges related to access and correcting misconceptions surrounding palliative care, the healthcare community can work towards ensuring that more patients receive timely and comprehensive palliative care services that align with their goals and values. Increased education, advocacy, and collaboration are essential in promoting the understanding and advancement of palliative care practices across diverse healthcare settings.
Future Directions in Palliative Care
As the field of palliative care continues to evolve, there are new advancements and changes shaping the landscape of how end-of-life care is provided. This section explores the latest advancements in palliative care and the evolving nature of palliative care services.
Advancements in Palliative Care
Advancements in palliative care are continually improving the quality of care provided to patients facing serious illnesses. These advancements encompass a range of areas, including pain management, symptom control, and holistic support for patients and their families.
One significant advancement in palliative care is the integration of telemedicine and telehealth services. This technology allows healthcare providers to connect with patients remotely, providing consultations, monitoring symptoms, and offering support from a distance. Telemedicine in palliative care enhances access to care for patients who may have mobility limitations or live in remote areas.
Another key advancement is the growing focus on personalized care plans tailored to individual patient needs. By taking a patient-centered approach, healthcare providers can deliver more effective and empathetic care that addresses the unique physical, emotional, and spiritual needs of each patient.
The Evolving Landscape of Palliative Care
The landscape of palliative care is continuously evolving to meet the changing needs of patients and families facing serious illnesses. One notable trend is the expansion of palliative care services beyond hospital settings into community-based settings, such as outpatient clinics and primary care offices.
There is also a growing recognition of the importance of early integration of palliative care alongside curative treatments for patients with life-limiting conditions. By incorporating palliative care earlier in the treatment process, patients can benefit from improved symptom management, enhanced communication with healthcare providers, and better quality of life throughout their illness trajectory.
Moreover, palliative care providers are increasingly collaborating with interdisciplinary teams to deliver comprehensive care that addresses not only the physical symptoms of illness but also the psychosocial, emotional, and spiritual aspects of care. This collaborative approach ensures that patients receive holistic and compassionate care that supports their well-being and dignity.
The future of palliative care holds promise for further advancements in care delivery, increased access to services, and a continued focus on enhancing the quality of life for patients facing serious illness. By staying abreast of these advancements and embracing the evolving landscape of palliative care, healthcare providers can ensure that patients receive the best possible care and support during challenging times.
Sources
https://media.capc.org/filer_public/68/bc/68bc93c7-14ad-4741-9830-8691729618d0/capc_press-kit.pdf
https://www.who.int/news-room/fact-sheets/detail/palliative-care
https://www.ncbi.nlm.nih.gov/books/NBK537113/













